Fallen Arches What To Look For
Overview

A fallen arch or flatfoot is known medically as pes planus. The foot loses the gently curving arch on the inner side of the sole, just in front of the heel. If this arch is flattened only when standing and returns when the foot is lifted off the ground, the condition is called flexible pes planus or flexible flatfoot. If the arch disappears in both foot positions, standing and elevated, the condition is called rigid pes planus or rigid flatfoot.
Causes
The arches of most individuals are fully developed by the age of 12 to 13. While some people are born with flat arches, for others, the arches fall over time. The tibial tendon, which runs along the inside of the ankle from above the ankle to the arch, can weaken with age and with heavy activity. The posterior tendon, main support structure for the arch, can become inflamed (tendonitis) or even tear if overloaded. For women, wearing high heels can affect the Achilles tendon and alter the structure and function of the ankle. The posterior tibial tendon may compensate for this stress and break down, causing the arches to fall. Obesity is another contributing factor, as well as a serious injury to the ankle or foot, arthritis and bad circulation such as occurs with diabetes.
Symptoms
A significant number of people with fallen arches (flat feet) experience no pain and have no problems. Some, however, may experience pain in their feet, especially when the connecting ligaments and muscles are strained. The leg joints may also be affected, resulting in pain. If the ankles turn inwards because of flat feet the most likely affected areas will be the feet, ankles and knees. Some people have flat feet because of a developmental fault during childhood, while others may find that the problem develops as they age, or after a pregnancy. There are some simple devices which may prevent the complications of flat feet.
Diagnosis
Your doctor examines your feet to determine two things, whether you have flat feet and the cause or causes. An exam may include the following steps, Checking your health history for evidence of illnesses or injuries that could be linked to flat feet or fallen arches, Looking at the soles of your shoes for unusual wear patterns, Observing the feet and legs as you stand and do simple movements, such as raising up on your toes, Testing the strength of muscles and tendons, including other tendons in the feet and legs, such as the Achilles tendon or the posterior tibial tendon, Taking X-rays or an MRI of your feet.
no-foot-pain.com
Non Surgical Treatment
The treatment is simple for flat feet. We will carry out a biomechanical assessment and full history, often along side a Computerised Gait Scan to give us an idea of how the foot is compensating. Treatment will be to, control how the foot hits the ground, support the middle of the foot and prevent the arch collapsing, promote normal movement in the front of the foot. The ability to do this will be dictated by the movement within the foot to start with. Treatment for all the above problems are often combined with a physiotherapy session in order to help develop a stretching and strengthening program for the back of the legs and the pelvis in order to allow normal function when the orthoses have been prescribed. If you are born with flat feet you will not grow out of them - if you get orthoses, like glasses you will need them for the rest of your life if you want to correct the mechanics in your foot. In 95% of cases, orthoses will reduce symptoms by at least 85%. In the other 5% we will work with them to get them to this level.
Surgical Treatment

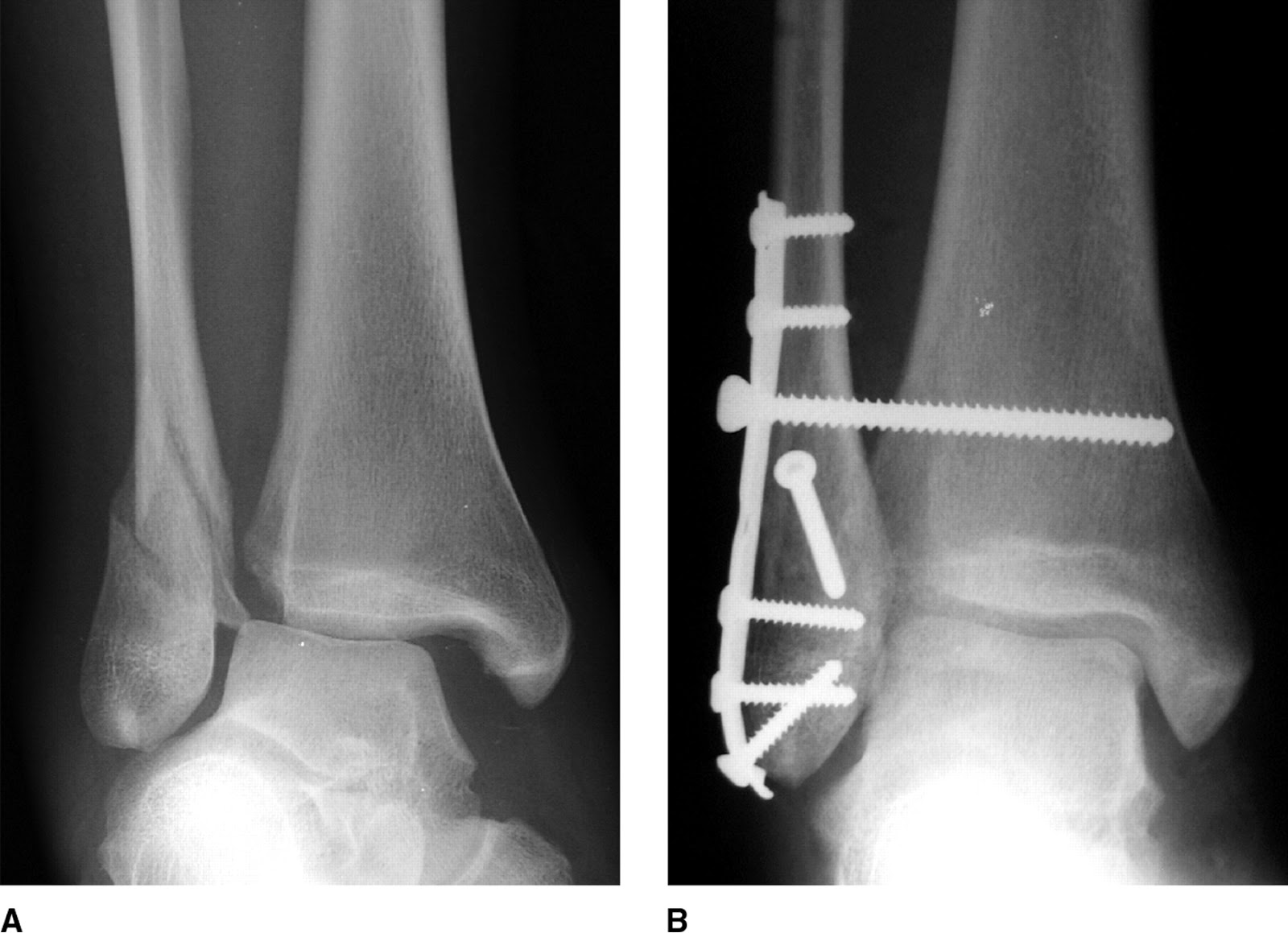
A combination of surgical procedures can be used to reconstruct the flatfoot. Generally, these procedures can be separated into those that correct deformities of the bones and those that repair ligaments and tendons. Your orthopaedic surgeon will choose the proper combination of procedures for your foot. Surgery of the foot can be performed under regional anesthesia, which is numbing the foot and ankle with a nerve or spinal block, or general anesthesia, which may require a breathing tube. A nerve block is often placed behind the knee to reduce pain after surgery.
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.

A fallen arch or flatfoot is known medically as pes planus. The foot loses the gently curving arch on the inner side of the sole, just in front of the heel. If this arch is flattened only when standing and returns when the foot is lifted off the ground, the condition is called flexible pes planus or flexible flatfoot. If the arch disappears in both foot positions, standing and elevated, the condition is called rigid pes planus or rigid flatfoot.
Causes
The arches of most individuals are fully developed by the age of 12 to 13. While some people are born with flat arches, for others, the arches fall over time. The tibial tendon, which runs along the inside of the ankle from above the ankle to the arch, can weaken with age and with heavy activity. The posterior tendon, main support structure for the arch, can become inflamed (tendonitis) or even tear if overloaded. For women, wearing high heels can affect the Achilles tendon and alter the structure and function of the ankle. The posterior tibial tendon may compensate for this stress and break down, causing the arches to fall. Obesity is another contributing factor, as well as a serious injury to the ankle or foot, arthritis and bad circulation such as occurs with diabetes.
Symptoms
A significant number of people with fallen arches (flat feet) experience no pain and have no problems. Some, however, may experience pain in their feet, especially when the connecting ligaments and muscles are strained. The leg joints may also be affected, resulting in pain. If the ankles turn inwards because of flat feet the most likely affected areas will be the feet, ankles and knees. Some people have flat feet because of a developmental fault during childhood, while others may find that the problem develops as they age, or after a pregnancy. There are some simple devices which may prevent the complications of flat feet.
Diagnosis
Your doctor examines your feet to determine two things, whether you have flat feet and the cause or causes. An exam may include the following steps, Checking your health history for evidence of illnesses or injuries that could be linked to flat feet or fallen arches, Looking at the soles of your shoes for unusual wear patterns, Observing the feet and legs as you stand and do simple movements, such as raising up on your toes, Testing the strength of muscles and tendons, including other tendons in the feet and legs, such as the Achilles tendon or the posterior tibial tendon, Taking X-rays or an MRI of your feet.
no-foot-pain.com
Non Surgical Treatment
The treatment is simple for flat feet. We will carry out a biomechanical assessment and full history, often along side a Computerised Gait Scan to give us an idea of how the foot is compensating. Treatment will be to, control how the foot hits the ground, support the middle of the foot and prevent the arch collapsing, promote normal movement in the front of the foot. The ability to do this will be dictated by the movement within the foot to start with. Treatment for all the above problems are often combined with a physiotherapy session in order to help develop a stretching and strengthening program for the back of the legs and the pelvis in order to allow normal function when the orthoses have been prescribed. If you are born with flat feet you will not grow out of them - if you get orthoses, like glasses you will need them for the rest of your life if you want to correct the mechanics in your foot. In 95% of cases, orthoses will reduce symptoms by at least 85%. In the other 5% we will work with them to get them to this level.
Surgical Treatment

A combination of surgical procedures can be used to reconstruct the flatfoot. Generally, these procedures can be separated into those that correct deformities of the bones and those that repair ligaments and tendons. Your orthopaedic surgeon will choose the proper combination of procedures for your foot. Surgery of the foot can be performed under regional anesthesia, which is numbing the foot and ankle with a nerve or spinal block, or general anesthesia, which may require a breathing tube. A nerve block is often placed behind the knee to reduce pain after surgery.
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.
Functional Leg Length Discrepancy Examination
Overview
Surgical operations to equalize leg lengths include the following. Shortening the longer leg. This is usually done if growth is already complete, and the patient is tall enough that losing an inch is not a problem. Slowing or stopping the growth of the longer leg. Growth of the lower limbs take place mainly in the epiphyseal plates (growth plates) of the lower femur and upper tibia and fibula. Stapling the growth plates in a child for a few years theoretically will stop growth for the period, and when the staples were removed, growth was supposed to resume. This procedure was quite popular till it was found that the amount of growth retarded was not certain, and when the staples where removed, the bone failed to resume its growth. Hence epiphyseal stapling has now been abandoned for the more reliable Epiphyseodesis. By use of modern fluoroscopic equipment, the surgeon can visualize the growth plate, and by making small incisions and using multiple drillings, the growth plate of the lower femur and/or upper tibia and fibula can be ablated. Since growth is stopped permanently by this procedure, the timing of the operation is crucial. This is probably the most commonly done procedure for correcting leg length discrepancy. But there is one limitation. The maximum amount of discrepancy that can be corrected by Epiphyseodesis is 5 cm. Lengthening the short leg. Various procedures have been done over the years to effect this result. External fixation devices are usually needed to hold the bone that is being lengthened. In the past, the bone to be lengthened was cut, and using the external fixation device, the leg was stretched out gradually over weeks. A gap in the bone was thus created, and a second operation was needed to place a bone block in the gap for stability and induce healing as a graft. More recently, a new technique called callotasis is being use. The bone to be lengthened is not cut completely, only partially and called a corticotomy. The bone is then distracted over an external device (usually an Ilizarov or Orthofix apparatus) very slowly so that bone healing is proceeding as the lengthening is being done. This avoids the need for a second procedure to insert bone graft. The procedure involved in leg lengthening is complicated, and fraught with risks. Theoretically, there is no limit to how much lengthening one can obtain, although the more ambitious one is, the higher the complication rate.
Causes
Leg length discrepancies can be caused by poor alignment of the pelvis or simply because one leg is structurally longer than the other. Regardless of the reason, your body wants to be symmetrical and will do its best to compensate for the length difference. The greater the leg length difference, the earlier the symptoms will present themselves to the patient. Specific diagnoses that coincide with leg length discrepancy include: scoliosis, lumbar herniated discs, sacroiliitis, pelvic obiliquity, greater trochanteric bursitis, hip arthritis, piriformis syndrome, patellofemoral syndrome and foot pronation. Other potential causes could be due to an injury (such as a fracture), bone disease, bone tumors, congenital problems (present at birth) or from a neuromuscular problem.
Symptoms
In addition to the distinctive walk of a person with leg length discrepancy, over time, other deformities may be noted, which help compensate for the condition. Toe walking on the short side to decrease the swaying during gait. The foot will supinate (high arch) on the shorter side. The foot will pronate (flattening of the arch) on the longer side. Excessive pronation leads to hypermobility and instability, resulting in metatarsus primus varus and associated unilateral juvenile hallux valgus (bunion) deformity.
Diagnosis
The doctor carefully examines the child. He or she checks to be sure the legs are actually different lengths. This is because problems with the hip (such as a loose joint) or back (scoliosis) can make the child appear to have one shorter leg, even though the legs are the same length. An X-ray of the child?s legs is taken. During the X-ray, a long ruler is put in the image so an accurate measurement of each leg bone can be taken. If an underlying cause of the discrepancy is suspected, tests are done to rule it out.
Non Surgical Treatment
Treatment is based on an estimate of how great the difference in leg length will be when the child grows up, Small differences (a half inch or less) do not need treatment. Differences of a half to one inch may require a lift inside the shoe.

leg length discrepancy test
Surgical Treatment
Lengthening is usually done by corticotomy and gradual distraction. This technique can result in lengthenings of 25% or more, but typically lengthening of 15%, or about 6 cm, is recommended. The limits of lengthening depend on patient tolerance, bony consolidation, maintenance of range of motion, and stability of the joints above and below the lengthened limb. Numerous fixation devices are available, such as the ring fixator with fine wires, monolateral fixator with half pins, or a hybrid frame. The choice of fixation device depends on the desired goal. A monolateral device is easier to apply and better tolerated by the patient. The disadvantages of monolateral fixation devices include the limitation of the degree of angular correction that can concurrently be obtained; the cantilever effect on the pins, which may result in angular deformity, especially when lengthening the femur in large patients; and the difficulty in making adjustments without placing new pins. Monolateral fixators appear to have a similar success rate as circular fixators, especially with more modest lengthenings (20%).
Surgical operations to equalize leg lengths include the following. Shortening the longer leg. This is usually done if growth is already complete, and the patient is tall enough that losing an inch is not a problem. Slowing or stopping the growth of the longer leg. Growth of the lower limbs take place mainly in the epiphyseal plates (growth plates) of the lower femur and upper tibia and fibula. Stapling the growth plates in a child for a few years theoretically will stop growth for the period, and when the staples were removed, growth was supposed to resume. This procedure was quite popular till it was found that the amount of growth retarded was not certain, and when the staples where removed, the bone failed to resume its growth. Hence epiphyseal stapling has now been abandoned for the more reliable Epiphyseodesis. By use of modern fluoroscopic equipment, the surgeon can visualize the growth plate, and by making small incisions and using multiple drillings, the growth plate of the lower femur and/or upper tibia and fibula can be ablated. Since growth is stopped permanently by this procedure, the timing of the operation is crucial. This is probably the most commonly done procedure for correcting leg length discrepancy. But there is one limitation. The maximum amount of discrepancy that can be corrected by Epiphyseodesis is 5 cm. Lengthening the short leg. Various procedures have been done over the years to effect this result. External fixation devices are usually needed to hold the bone that is being lengthened. In the past, the bone to be lengthened was cut, and using the external fixation device, the leg was stretched out gradually over weeks. A gap in the bone was thus created, and a second operation was needed to place a bone block in the gap for stability and induce healing as a graft. More recently, a new technique called callotasis is being use. The bone to be lengthened is not cut completely, only partially and called a corticotomy. The bone is then distracted over an external device (usually an Ilizarov or Orthofix apparatus) very slowly so that bone healing is proceeding as the lengthening is being done. This avoids the need for a second procedure to insert bone graft. The procedure involved in leg lengthening is complicated, and fraught with risks. Theoretically, there is no limit to how much lengthening one can obtain, although the more ambitious one is, the higher the complication rate.

Causes
Leg length discrepancies can be caused by poor alignment of the pelvis or simply because one leg is structurally longer than the other. Regardless of the reason, your body wants to be symmetrical and will do its best to compensate for the length difference. The greater the leg length difference, the earlier the symptoms will present themselves to the patient. Specific diagnoses that coincide with leg length discrepancy include: scoliosis, lumbar herniated discs, sacroiliitis, pelvic obiliquity, greater trochanteric bursitis, hip arthritis, piriformis syndrome, patellofemoral syndrome and foot pronation. Other potential causes could be due to an injury (such as a fracture), bone disease, bone tumors, congenital problems (present at birth) or from a neuromuscular problem.
Symptoms
In addition to the distinctive walk of a person with leg length discrepancy, over time, other deformities may be noted, which help compensate for the condition. Toe walking on the short side to decrease the swaying during gait. The foot will supinate (high arch) on the shorter side. The foot will pronate (flattening of the arch) on the longer side. Excessive pronation leads to hypermobility and instability, resulting in metatarsus primus varus and associated unilateral juvenile hallux valgus (bunion) deformity.
Diagnosis
The doctor carefully examines the child. He or she checks to be sure the legs are actually different lengths. This is because problems with the hip (such as a loose joint) or back (scoliosis) can make the child appear to have one shorter leg, even though the legs are the same length. An X-ray of the child?s legs is taken. During the X-ray, a long ruler is put in the image so an accurate measurement of each leg bone can be taken. If an underlying cause of the discrepancy is suspected, tests are done to rule it out.
Non Surgical Treatment
Treatment is based on an estimate of how great the difference in leg length will be when the child grows up, Small differences (a half inch or less) do not need treatment. Differences of a half to one inch may require a lift inside the shoe.

leg length discrepancy test
Surgical Treatment
Lengthening is usually done by corticotomy and gradual distraction. This technique can result in lengthenings of 25% or more, but typically lengthening of 15%, or about 6 cm, is recommended. The limits of lengthening depend on patient tolerance, bony consolidation, maintenance of range of motion, and stability of the joints above and below the lengthened limb. Numerous fixation devices are available, such as the ring fixator with fine wires, monolateral fixator with half pins, or a hybrid frame. The choice of fixation device depends on the desired goal. A monolateral device is easier to apply and better tolerated by the patient. The disadvantages of monolateral fixation devices include the limitation of the degree of angular correction that can concurrently be obtained; the cantilever effect on the pins, which may result in angular deformity, especially when lengthening the femur in large patients; and the difficulty in making adjustments without placing new pins. Monolateral fixators appear to have a similar success rate as circular fixators, especially with more modest lengthenings (20%).
All The Things You Should Know About
Overview

The most common cause of heel pain is plantar fasciitis which is commonly referred to as a heel spur. Plantar fascia is a broad band of fibrous tissue which runs along the bottom surface of the foot, from the heel to the toes. Plantar fasciitis is a condition in which the plantar fascia is inflamed. This condition can be very painful and cause a considerable amount of suffering.
Causes
Achilles tendon rupture, the tendon of the heel cord behind the ankle is torn. Bone bruise. Bone cyst, a solitary fluid-filled cyst (cavity) in a bone. Gout, levels of uric acid in the blood rise until the level becomes excessive (hyperuricemia), causing urate crystals to build up around the joints. This causes inflammation and severe pain when a gout attack happens. Neuroma (Morton's neuroma) a swollen nerve in the ball of the foot, commonly between the base of the second and third toes. Osteomyelitis , osteomyelitis means infection of the bone or bone marrow; inflammation of the bone due to infection. Osteomyelitis sometimes occurs as a complication of injury or surgery. In some cases, the infection may get into bone tissue from the bloodstream. Patients with osteomyelitis typically experience deep pain and muscle spasms in the inflammation area, as well as fever. Peripheral neuropathy, neuropathy is a collection of disorders that occurs when nerves of the peripheral nervous system (the part of the nervous system outside of the brain and spinal cord) are damaged. The condition is generally referred to as peripheral neuropathy, and it is most commonly due to damage to nerve axons. Neuropathy usually causes pain and numbness in the hands and feet. It can result from traumatic injuries, infections, metabolic disorders and exposure to toxins. One of the most common causes of neuropathy is diabetes. Problems with your gait, wrong posture when walking/running. Rheumatoid arthritis, rheumatoid arthritis, sometimes referred to as rheumatoid disease, is a chronic (long lasting), progressive and disabling auto-immune disease condition that causes inflammation and pain in the joints, the tissue around the joints, and other organs in the human body. Rheumatoid arthritis usually affects the joints in the hands and feet first, but any joint may become affected. Patients with rheumatoid arthritis commonly have stiff joints and feel generally unwell and tired.
Symptoms
The symptoms of plantar fasciitis include pain along the inside edge of the heel near the arch of the foot. The pain is worse when weight is placed on the foot especially after a long period of rest or inactivity. This is usually most pronounced in the morning when the foot is first placed on the floor. This symptom called first-step pain is typical of plantar fasciitis. Prolonged standing can also increase the painful symptoms. It may feel better after activity but most patients report increased pain by the end of the day. Pressing on this part of the heel causes tenderness. Pulling the toes back toward the face can be very painful.
Diagnosis
The diagnosis of plantar fasciitis is generally made during the history and physical examination. There are several conditions that can cause heel pain, and plantar fasciitis must be distinguished from these conditions. Pain can be referred to the heel and foot from other areas of the body such as the low back, hip, knee, and/or ankle. Special tests to challenge these areas are performed to help confirm the problem is truly coming from the plantar fascia. An X-ray may be ordered to rule out a stress fracture of the heel bone and to see if a bone spur is present that is large enough to cause problems. Other helpful imaging studies include bone scans, MRI, and ultrasound. Ultrasonographic exam may be favored as it is quick, less expensive, and does not expose you to radiation. Laboratory investigation may be necessary in some cases to rule out a systemic illness causing the heel pain, such as rheumatoid arthritis, Reiter's syndrome, or ankylosing spondylitis. These are diseases that affect the entire body but may show up at first as pain in the heel.
Non Surgical Treatment
Most patients get better with the help of nonsurgical treatments. Stretches for the calf muscles on the back of the lower leg take tension off the plantar fascia. A night splint can be worn while you sleep. The night splint keeps your foot from bending downward. It places a mild stretch on the calf muscles and the plantar fascia. Some people seem to get better faster when using a night splint. They report having less heel pain when placing the sore foot on the ground in the morning. There have been a few studies that reported no significant benefit from adding night splinting to a program of antiinflammatory meds and stretching. Other studies report the benefits of short-term casting to unload the heel, immobilize the plantar fascia, and reduce repetitive microtrauma. Supporting the arch with a well fitted arch support, or orthotic, may also help reduce pressure on the plantar fascia. Placing a special type of insert into the shoe, called a heel cup, can reduce the pressure on the sore area. Wearing a silicone heel pad adds cushion to a heel that has lost some of the fat pad through degeneration. Shock wave therapy is a newer form of nonsurgical treatment. It uses a machine to generate shock wave pulses to the sore area. Patients generally receive the treatment once each week for up to three weeks. It is not known exactly why it works for plantar fasciitis. It's possible that the shock waves disrupt the plantar fascial tissue enough to start a healing response. The resulting release of local growth factors and stem cells causes an increase in blood flow to the area. Recent studies indicate that this form of treatment can help ease pain, while improving range of motion and function.
Surgical Treatment
With the advancements in technology and treatments, if you do need to have surgery for the heel, it is very minimal incision that?s done. And the nice thing is your recovery period is short and you should be able to bear weight right after the surgery. This means you can get back to your weekly routine in just a few weeks. Recovery is a lot different than it used to be and a lot of it is because of doing a minimal incision and decreasing trauma to soft tissues, as well as even the bone. So if you need surgery, then your recovery period is pretty quick.
heel cushions for plantar fasciitis
Prevention

It may not be possible to prevent all cases of heel pain. However, there are some easy steps that you can take to avoid injury to the heel and prevent pain. Whenever possible, you should wear shoes that fit properly and support the foot, wear the right shoes for physical activity, stretch your muscles before exercising, pace yourself during physical activity, maintain a healthy diet, rest when you feel tired or when your muscles ache, maintain a healthy weight.

The most common cause of heel pain is plantar fasciitis which is commonly referred to as a heel spur. Plantar fascia is a broad band of fibrous tissue which runs along the bottom surface of the foot, from the heel to the toes. Plantar fasciitis is a condition in which the plantar fascia is inflamed. This condition can be very painful and cause a considerable amount of suffering.
Causes
Achilles tendon rupture, the tendon of the heel cord behind the ankle is torn. Bone bruise. Bone cyst, a solitary fluid-filled cyst (cavity) in a bone. Gout, levels of uric acid in the blood rise until the level becomes excessive (hyperuricemia), causing urate crystals to build up around the joints. This causes inflammation and severe pain when a gout attack happens. Neuroma (Morton's neuroma) a swollen nerve in the ball of the foot, commonly between the base of the second and third toes. Osteomyelitis , osteomyelitis means infection of the bone or bone marrow; inflammation of the bone due to infection. Osteomyelitis sometimes occurs as a complication of injury or surgery. In some cases, the infection may get into bone tissue from the bloodstream. Patients with osteomyelitis typically experience deep pain and muscle spasms in the inflammation area, as well as fever. Peripheral neuropathy, neuropathy is a collection of disorders that occurs when nerves of the peripheral nervous system (the part of the nervous system outside of the brain and spinal cord) are damaged. The condition is generally referred to as peripheral neuropathy, and it is most commonly due to damage to nerve axons. Neuropathy usually causes pain and numbness in the hands and feet. It can result from traumatic injuries, infections, metabolic disorders and exposure to toxins. One of the most common causes of neuropathy is diabetes. Problems with your gait, wrong posture when walking/running. Rheumatoid arthritis, rheumatoid arthritis, sometimes referred to as rheumatoid disease, is a chronic (long lasting), progressive and disabling auto-immune disease condition that causes inflammation and pain in the joints, the tissue around the joints, and other organs in the human body. Rheumatoid arthritis usually affects the joints in the hands and feet first, but any joint may become affected. Patients with rheumatoid arthritis commonly have stiff joints and feel generally unwell and tired.
Symptoms
The symptoms of plantar fasciitis include pain along the inside edge of the heel near the arch of the foot. The pain is worse when weight is placed on the foot especially after a long period of rest or inactivity. This is usually most pronounced in the morning when the foot is first placed on the floor. This symptom called first-step pain is typical of plantar fasciitis. Prolonged standing can also increase the painful symptoms. It may feel better after activity but most patients report increased pain by the end of the day. Pressing on this part of the heel causes tenderness. Pulling the toes back toward the face can be very painful.
Diagnosis
The diagnosis of plantar fasciitis is generally made during the history and physical examination. There are several conditions that can cause heel pain, and plantar fasciitis must be distinguished from these conditions. Pain can be referred to the heel and foot from other areas of the body such as the low back, hip, knee, and/or ankle. Special tests to challenge these areas are performed to help confirm the problem is truly coming from the plantar fascia. An X-ray may be ordered to rule out a stress fracture of the heel bone and to see if a bone spur is present that is large enough to cause problems. Other helpful imaging studies include bone scans, MRI, and ultrasound. Ultrasonographic exam may be favored as it is quick, less expensive, and does not expose you to radiation. Laboratory investigation may be necessary in some cases to rule out a systemic illness causing the heel pain, such as rheumatoid arthritis, Reiter's syndrome, or ankylosing spondylitis. These are diseases that affect the entire body but may show up at first as pain in the heel.
Non Surgical Treatment
Most patients get better with the help of nonsurgical treatments. Stretches for the calf muscles on the back of the lower leg take tension off the plantar fascia. A night splint can be worn while you sleep. The night splint keeps your foot from bending downward. It places a mild stretch on the calf muscles and the plantar fascia. Some people seem to get better faster when using a night splint. They report having less heel pain when placing the sore foot on the ground in the morning. There have been a few studies that reported no significant benefit from adding night splinting to a program of antiinflammatory meds and stretching. Other studies report the benefits of short-term casting to unload the heel, immobilize the plantar fascia, and reduce repetitive microtrauma. Supporting the arch with a well fitted arch support, or orthotic, may also help reduce pressure on the plantar fascia. Placing a special type of insert into the shoe, called a heel cup, can reduce the pressure on the sore area. Wearing a silicone heel pad adds cushion to a heel that has lost some of the fat pad through degeneration. Shock wave therapy is a newer form of nonsurgical treatment. It uses a machine to generate shock wave pulses to the sore area. Patients generally receive the treatment once each week for up to three weeks. It is not known exactly why it works for plantar fasciitis. It's possible that the shock waves disrupt the plantar fascial tissue enough to start a healing response. The resulting release of local growth factors and stem cells causes an increase in blood flow to the area. Recent studies indicate that this form of treatment can help ease pain, while improving range of motion and function.
Surgical Treatment
With the advancements in technology and treatments, if you do need to have surgery for the heel, it is very minimal incision that?s done. And the nice thing is your recovery period is short and you should be able to bear weight right after the surgery. This means you can get back to your weekly routine in just a few weeks. Recovery is a lot different than it used to be and a lot of it is because of doing a minimal incision and decreasing trauma to soft tissues, as well as even the bone. So if you need surgery, then your recovery period is pretty quick.
heel cushions for plantar fasciitis
Prevention

It may not be possible to prevent all cases of heel pain. However, there are some easy steps that you can take to avoid injury to the heel and prevent pain. Whenever possible, you should wear shoes that fit properly and support the foot, wear the right shoes for physical activity, stretch your muscles before exercising, pace yourself during physical activity, maintain a healthy diet, rest when you feel tired or when your muscles ache, maintain a healthy weight.
Coping with Mortons Neuroma
Overview
 Morton's neuroma, also called Morton's metatarsalgia, Morton's disease, Morton's neuralgia, Morton metatarsalgia, Morton nerve entrapment, plantar neuroma, or intermetatarsal neuroma is a benign (non-cancerous) growth of nerve tissue (neuroma) that develops in the foot, usually between the third and fourth toes (an intermetatarsal plantar nerve, most commonly of the third and fourth intermetatarsal spaces). It is a common, painful condition.
Morton's neuroma, also called Morton's metatarsalgia, Morton's disease, Morton's neuralgia, Morton metatarsalgia, Morton nerve entrapment, plantar neuroma, or intermetatarsal neuroma is a benign (non-cancerous) growth of nerve tissue (neuroma) that develops in the foot, usually between the third and fourth toes (an intermetatarsal plantar nerve, most commonly of the third and fourth intermetatarsal spaces). It is a common, painful condition.
Causes
Anything that causes compression or irritation of the nerve can lead to the development of a neuroma. One of the most common offenders is wearing shoes that have a tapered toe box, or high-heeled shoes that cause the toes to be forced into the toe box. People with certain foot deformities - bunions, hammertoes, flatfeet, or more flexible feet - are at higher risk for developing a neuroma. Other potential causes are activities that involve repetitive irritation to the ball of the foot, such as running or court sports. An injury or other type of trauma to the area may also lead to a neuroma.
Symptoms
Patients will often experience a clicking feeling in the forefoot followed by a sharp shooting pain or a sensation of numbness or pins and needles extending into ends of their toes. Tight narrow fitting shoes may often exacerbate these feelings which become worse after long periods of standing or walking. Once the Mortons nueroma progresses symptoms will become more frequent and often more intense.
Diagnosis
The physician will make the diagnosis of Morton's neuroma based upon the patient's symptoms as described above in an interview, or history, and a physical examination. The physical examination will reveal exceptional tenderness in the involved interspace when the nerve area is pressed on the bottom of the foot. As the interspace is palpated, and pressure is applied from the top to the bottom of the foot, a click can sometimes be felt which reproduces the patient's pain. This is known as a Mulder's sign. Because of inconsistent results, imaging studies such as MRI or ultrasound scanning are not useful diagnostic tools for Morton's neuroma. Thus the physician must rely exclusively on the patient's history and physical examination in order to make a diagnosis.
Non Surgical Treatment
Properly resting the foot in addition to the use of appropriate footwear including, as necessary, pads and arch supports, often brings relief from Morton?s Neuroma, without resorting to surgery. A physician may also recommend anti-inflammatory drugs, cortisone injections and, should the condition fail to resolve itself, surgery.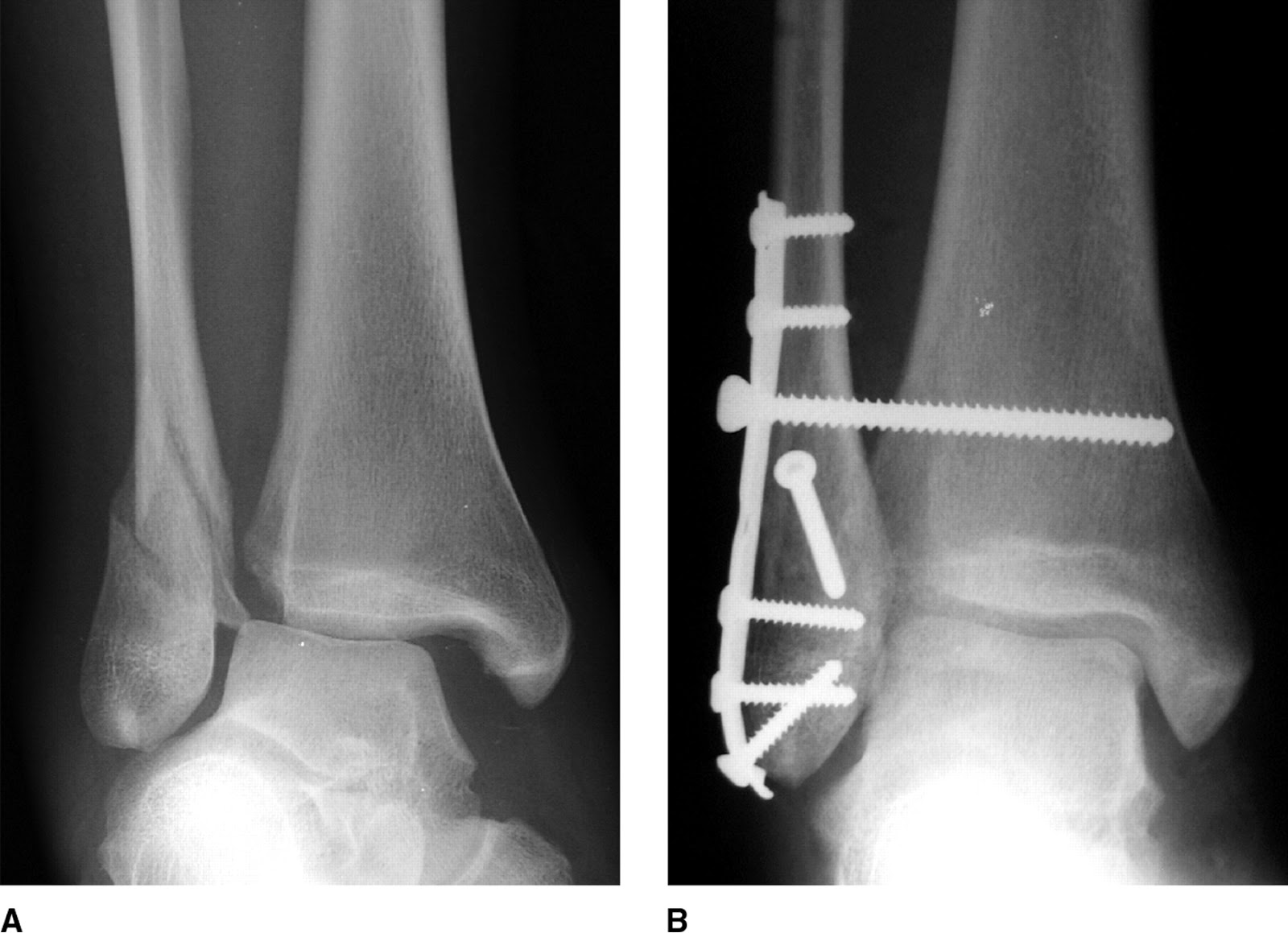
Surgical Treatment
Surgery for mortons neuroma consists of either a decompression, where more space is created for the nerve or a resection, where this part of the nerve is removed completely. This will result in some permanent minor numbness. Success rates for surgical procedures to treat mortons neuroma have a high success rate.
Prevention
Women, particularly those who wear tight shoes, are at greatest risk for Morton?s neuroma. The best way to prevent the condition is to wear shoes with wide toe boxes. Tight, pointed shoes squeeze bones, ligaments, muscles and nerves. High heels may worsen the problem by shifting your weight forward. Over time, this combination can cause the nerves to swell and become painful.
 Morton's neuroma, also called Morton's metatarsalgia, Morton's disease, Morton's neuralgia, Morton metatarsalgia, Morton nerve entrapment, plantar neuroma, or intermetatarsal neuroma is a benign (non-cancerous) growth of nerve tissue (neuroma) that develops in the foot, usually between the third and fourth toes (an intermetatarsal plantar nerve, most commonly of the third and fourth intermetatarsal spaces). It is a common, painful condition.
Morton's neuroma, also called Morton's metatarsalgia, Morton's disease, Morton's neuralgia, Morton metatarsalgia, Morton nerve entrapment, plantar neuroma, or intermetatarsal neuroma is a benign (non-cancerous) growth of nerve tissue (neuroma) that develops in the foot, usually between the third and fourth toes (an intermetatarsal plantar nerve, most commonly of the third and fourth intermetatarsal spaces). It is a common, painful condition.Causes
Anything that causes compression or irritation of the nerve can lead to the development of a neuroma. One of the most common offenders is wearing shoes that have a tapered toe box, or high-heeled shoes that cause the toes to be forced into the toe box. People with certain foot deformities - bunions, hammertoes, flatfeet, or more flexible feet - are at higher risk for developing a neuroma. Other potential causes are activities that involve repetitive irritation to the ball of the foot, such as running or court sports. An injury or other type of trauma to the area may also lead to a neuroma.
Symptoms
Patients will often experience a clicking feeling in the forefoot followed by a sharp shooting pain or a sensation of numbness or pins and needles extending into ends of their toes. Tight narrow fitting shoes may often exacerbate these feelings which become worse after long periods of standing or walking. Once the Mortons nueroma progresses symptoms will become more frequent and often more intense.
Diagnosis
The physician will make the diagnosis of Morton's neuroma based upon the patient's symptoms as described above in an interview, or history, and a physical examination. The physical examination will reveal exceptional tenderness in the involved interspace when the nerve area is pressed on the bottom of the foot. As the interspace is palpated, and pressure is applied from the top to the bottom of the foot, a click can sometimes be felt which reproduces the patient's pain. This is known as a Mulder's sign. Because of inconsistent results, imaging studies such as MRI or ultrasound scanning are not useful diagnostic tools for Morton's neuroma. Thus the physician must rely exclusively on the patient's history and physical examination in order to make a diagnosis.
Non Surgical Treatment
Properly resting the foot in addition to the use of appropriate footwear including, as necessary, pads and arch supports, often brings relief from Morton?s Neuroma, without resorting to surgery. A physician may also recommend anti-inflammatory drugs, cortisone injections and, should the condition fail to resolve itself, surgery.
Surgical Treatment
Surgery for mortons neuroma consists of either a decompression, where more space is created for the nerve or a resection, where this part of the nerve is removed completely. This will result in some permanent minor numbness. Success rates for surgical procedures to treat mortons neuroma have a high success rate.
Prevention
Women, particularly those who wear tight shoes, are at greatest risk for Morton?s neuroma. The best way to prevent the condition is to wear shoes with wide toe boxes. Tight, pointed shoes squeeze bones, ligaments, muscles and nerves. High heels may worsen the problem by shifting your weight forward. Over time, this combination can cause the nerves to swell and become painful.
For Leg Length Discrepancy Chiropodists Prefer Shoe Lifts
There are two different kinds of leg length discrepancies, congenital and acquired. Congenital means you are born with it. One leg is anatomically shorter than the other. As a result of developmental stages of aging, the brain picks up on the gait pattern and identifies some variation. The body typically adapts by dipping one shoulder to the "short" side. A difference of less than a quarter inch isn't really uncommon, demand Shoe Lifts to compensate and in most cases won't have a profound effect over a lifetime.

Leg length inequality goes typically undiscovered on a daily basis, yet this condition is very easily fixed, and can eliminate quite a few incidents of back ache.
Treatment for leg length inequality commonly consists of Shoe Lifts. These are cost-effective, usually priced at less than twenty dollars, compared to a custom orthotic of $200 and up. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Chronic back pain is the most prevalent condition afflicting people today. Over 80 million men and women have problems with back pain at some stage in their life. It is a problem that costs employers millions of dollars annually on account of lost time and productivity. Fresh and superior treatment methods are constantly sought after in the hope of lowering economic impact this issue causes.

People from all corners of the world suffer from foot ache as a result of leg length discrepancy. In these types of cases Shoe Lifts might be of very helpful. The lifts are capable of alleviating any discomfort in the feet. Shoe Lifts are recommended by many expert orthopaedic practitioners".
So that you can support the body in a healthy and balanced fashion, your feet have a vital role to play. Despite that, it is sometimes the most neglected zone in the body. Many people have flat-feet which means there may be unequal force exerted on the feet. This causes other areas of the body including knees, ankles and backs to be impacted too. Shoe Lifts guarantee that correct posture and balance are restored.

Leg length inequality goes typically undiscovered on a daily basis, yet this condition is very easily fixed, and can eliminate quite a few incidents of back ache.
Treatment for leg length inequality commonly consists of Shoe Lifts. These are cost-effective, usually priced at less than twenty dollars, compared to a custom orthotic of $200 and up. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Chronic back pain is the most prevalent condition afflicting people today. Over 80 million men and women have problems with back pain at some stage in their life. It is a problem that costs employers millions of dollars annually on account of lost time and productivity. Fresh and superior treatment methods are constantly sought after in the hope of lowering economic impact this issue causes.

People from all corners of the world suffer from foot ache as a result of leg length discrepancy. In these types of cases Shoe Lifts might be of very helpful. The lifts are capable of alleviating any discomfort in the feet. Shoe Lifts are recommended by many expert orthopaedic practitioners".
So that you can support the body in a healthy and balanced fashion, your feet have a vital role to play. Despite that, it is sometimes the most neglected zone in the body. Many people have flat-feet which means there may be unequal force exerted on the feet. This causes other areas of the body including knees, ankles and backs to be impacted too. Shoe Lifts guarantee that correct posture and balance are restored.
Treating Leg Length Imbalances With Shoe Lifts
There are two different kinds of leg length discrepancies, congenital and acquired. Congenital indicates that you are born with it. One leg is anatomically shorter compared to the other. As a result of developmental phases of aging, the human brain senses the stride pattern and recognizes some difference. Your body usually adapts by dipping one shoulder to the "short" side. A difference of less than a quarter inch is not grossly abnormal, doesn't need Shoe Lifts to compensate and normally won't have a serious effect over a lifetime.

Leg length inequality goes typically undiscovered on a daily basis, however this problem is simply corrected, and can eradicate numerous instances of upper back pain.
Therapy for leg length inequality commonly consists of Shoe Lifts. These are generally affordable, frequently being under twenty dollars, in comparison to a custom orthotic of $200 plus. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Back ache is easily the most prevalent ailment impacting men and women today. Around 80 million people are affected by back pain at some point in their life. It's a problem which costs companies huge amounts of money annually on account of time lost and output. Fresh and improved treatment methods are always sought after in the hope of lowering economical influence this issue causes.

Men and women from all corners of the world suffer from foot ache as a result of leg length discrepancy. In these situations Shoe Lifts might be of immense help. The lifts are capable of alleviating any pain in the feet. Shoe Lifts are recommended by numerous expert orthopaedic physicians.
In order to support the human body in a well balanced fashion, your feet have a crucial part to play. Despite that, it can be the most neglected region of the human body. Some people have flat-feet meaning there may be unequal force placed on the feet. This causes other areas of the body such as knees, ankles and backs to be affected too. Shoe Lifts guarantee that proper posture and balance are restored.

Leg length inequality goes typically undiscovered on a daily basis, however this problem is simply corrected, and can eradicate numerous instances of upper back pain.
Therapy for leg length inequality commonly consists of Shoe Lifts. These are generally affordable, frequently being under twenty dollars, in comparison to a custom orthotic of $200 plus. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Back ache is easily the most prevalent ailment impacting men and women today. Around 80 million people are affected by back pain at some point in their life. It's a problem which costs companies huge amounts of money annually on account of time lost and output. Fresh and improved treatment methods are always sought after in the hope of lowering economical influence this issue causes.

Men and women from all corners of the world suffer from foot ache as a result of leg length discrepancy. In these situations Shoe Lifts might be of immense help. The lifts are capable of alleviating any pain in the feet. Shoe Lifts are recommended by numerous expert orthopaedic physicians.
In order to support the human body in a well balanced fashion, your feet have a crucial part to play. Despite that, it can be the most neglected region of the human body. Some people have flat-feet meaning there may be unequal force placed on the feet. This causes other areas of the body such as knees, ankles and backs to be affected too. Shoe Lifts guarantee that proper posture and balance are restored.
For Leg Length Difference Chiropodists Prefer Shoe Lifts
There are two unique variations of leg length discrepancies, congenital and acquired. Congenital indicates you are born with it. One leg is structurally shorter in comparison to the other. As a result of developmental stages of aging, the human brain senses the walking pattern and identifies some variance. The entire body typically adapts by tilting one shoulder over to the "short" side. A difference of under a quarter inch is not grossly irregular, doesn't need Shoe Lifts to compensate and mostly won't have a serious effect over a lifetime.

Leg length inequality goes mainly undiagnosed on a daily basis, however this problem is simply solved, and can reduce quite a few instances of upper back pain.
Treatment for leg length inequality typically consists of Shoe Lifts. These are typically cost-effective, often priced at below twenty dollars, in comparison to a custom orthotic of $200 or more. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Chronic back pain is easily the most common health problem affecting men and women today. Over 80 million people are affected by back pain at some point in their life. It is a problem that costs companies millions of dollars each year on account of lost time and production. New and improved treatment methods are constantly sought after in the hope of reducing the economical impact this issue causes.

Men and women from all corners of the earth experience foot ache as a result of leg length discrepancy. In a lot of these cases Shoe Lifts can be of very beneficial. The lifts are capable of alleviating any pain and discomfort in the feet. Shoe Lifts are recommended by countless qualified orthopaedic orthopedists.
To be able to support the body in a well-balanced manner, feet have a vital job to play. Despite that, it's often the most overlooked region of the human body. Many people have flat-feet which means there may be unequal force exerted on the feet. This will cause other parts of the body including knees, ankles and backs to be impacted too. Shoe Lifts guarantee that ideal posture and balance are restored.

Leg length inequality goes mainly undiagnosed on a daily basis, however this problem is simply solved, and can reduce quite a few instances of upper back pain.
Treatment for leg length inequality typically consists of Shoe Lifts. These are typically cost-effective, often priced at below twenty dollars, in comparison to a custom orthotic of $200 or more. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Chronic back pain is easily the most common health problem affecting men and women today. Over 80 million people are affected by back pain at some point in their life. It is a problem that costs companies millions of dollars each year on account of lost time and production. New and improved treatment methods are constantly sought after in the hope of reducing the economical impact this issue causes.

Men and women from all corners of the earth experience foot ache as a result of leg length discrepancy. In a lot of these cases Shoe Lifts can be of very beneficial. The lifts are capable of alleviating any pain and discomfort in the feet. Shoe Lifts are recommended by countless qualified orthopaedic orthopedists.
To be able to support the body in a well-balanced manner, feet have a vital job to play. Despite that, it's often the most overlooked region of the human body. Many people have flat-feet which means there may be unequal force exerted on the feet. This will cause other parts of the body including knees, ankles and backs to be impacted too. Shoe Lifts guarantee that ideal posture and balance are restored.